Molina Healthcare of Michigan Medicare Prior Authorization Request Form 2013 free printable template
Show details
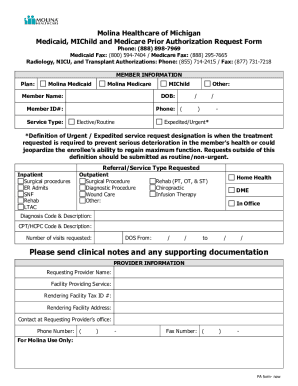
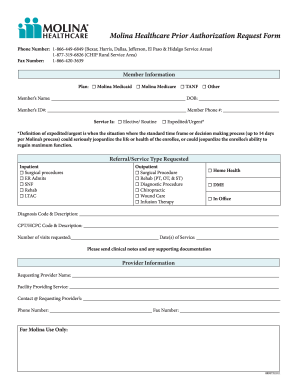
Molina Healthcare of Michigan Prior Authorization Request Form Phone Number 888 898-7969 Medicaid Fax Number 800 594-7404 Medicare Fax 888 295-7665 Member Information Plan Molina Medicaid Molina MIChild Member Name Other DOB Member ID Member Phone Service Is Elective/Routine Expedited/Urgent Definition of Urgent / Expedited service request designation is when the treatment requested is required to prevent serious deterioration in the member s hea...
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign
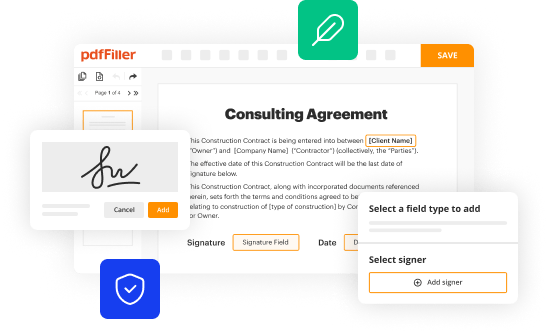
Edit your molina prior authorization form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your molina prior authorization form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit molina prior authorization form online
Use the instructions below to start using our professional PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit molina prior authorization form michigan. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. Then click Done when you're done editing and go to the Documents tab to merge or split the file. If you want to lock or unlock the file, click the lock or unlock button.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
With pdfFiller, dealing with documents is always straightforward.
Molina Healthcare of Michigan Medicare Prior Authorization Request Form Form Versions
Version
Form Popularity
Fillable & printabley
4.5 Satisfied (54 Votes)
4.0 Satisfied (40 Votes)
How to fill out molina prior authorization form
How to fill out Molina prior authorization form:
01
Obtain the Molina prior authorization form from the provider or download it from their website.
02
Fill out your personal information, including your name, address, contact information, and Molina member ID number.
03
Provide the relevant details of the requested medical service, such as the diagnosis, procedure codes, and any supporting documentation.
04
Include the healthcare professional's information, such as their name, contact details, and NPI number.
05
Fill out any additional required information, such as the date of the service, expected length of treatment, and any applicable medication information.
06
Review the form for accuracy and completeness before submitting it to Molina for prior authorization.
Who needs Molina prior authorization form:
01
Patients who have health insurance coverage with Molina and need a medical service or procedure that requires prior authorization.
02
Healthcare professionals who are part of the Molina network and are requesting prior authorization for their patients' medical services or procedures.
Fill molina medicaid prior authorization : Try Risk Free
People Also Ask about molina prior authorization form
What type insurance is Molina Healthcare of California?
Is Molina WA Medicaid?
Is Molina Healthcare the same as Medi Cal?
How do I contact Molina Healthcare Texas?
Is Molina Healthcare under Medi-Cal?
How do you contact Availity?
Why are prior authorizations so difficult?
What is the difference between Molina and medical?
How do you extend authorization of Availity?
What is the difference between Molina and Medi-Cal?
What is Washington's Medicaid called?
What is the difference between Availity and Availity essentials?
Is Molina Healthcare of Texas Medicare?
Is Washington State medical Medicaid or Medicare?
Is Molina Healthcare of Texas Medicaid?
Is Molina Healthcare of Washington Medicare or Medicaid?
What is another name for Molina Healthcare?
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How to fill out molina prior authorization form?
1. Start by completing the patient information section of the form. Include the patient's name, date of birth, address, phone number, and other contact information.
2. Indicate the prescribing physician's contact information.
3. Describe the medication for which prior authorization is being requested. Include the name, dosage, quantity, and frequency of administration.
4. Provide information about the diagnosis that the medication is intended to treat. Include the diagnosis code and any other pertinent clinical information.
5. List any other medications that the patient is currently taking.
6. Sign and date the form.
7. Submit the form to Molina for review and processing.
What is the penalty for the late filing of molina prior authorization form?
Typically, when a Molina Prior Authorization form is submitted late, there is no specific penalty applied. However, the submission may be denied due to the delay, and any services rendered prior to the authorization may not be eligible for reimbursement.
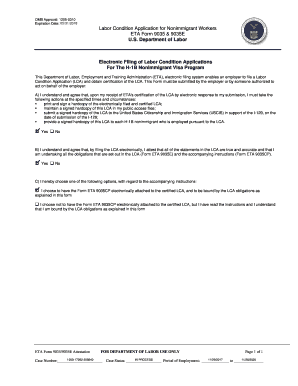
What is molina prior authorization form?
Molina Healthcare is a managed care company that provides health insurance plans for individuals and families. A prior authorization form is a document required by insurance companies to request coverage for certain medications, procedures, or treatments.
A Molina prior authorization form is a specific form used by Molina Healthcare to review and approve or deny requests for coverage prior to the services being provided. This is done to ensure that the requested service is medically necessary and meets the criteria set by the insurance company.
The form usually requires the healthcare provider to provide detailed information about the patient's medical condition, the proposed treatment or medication, and supporting documentation such as clinical notes or test results. The completed form is then submitted to Molina for review, and a decision is made on whether to approve or deny the requested coverage.
Who is required to file molina prior authorization form?
The individuals who are required to file a Molina prior authorization form are healthcare providers, medical practices, or hospitals who want to request approval from Molina Healthcare, an insurance provider, for certain medical services, procedures, or medications that may require prior authorization.
What is the purpose of molina prior authorization form?
The purpose of the Molina prior authorization form is to request approval from Molina Healthcare, a managed care company, for certain medications, treatments, procedures, or services before they are provided. It helps ensure that the requested healthcare services are medically necessary and covered by the insurance plan, thus preventing unnecessary expenses for both the patient and the insurance provider. The form requires relevant information about the patient, provider, and the requested service, which is then reviewed by Molina to make a determination regarding coverage.
What information must be reported on molina prior authorization form?
The specific information that must be reported on a Molina prior authorization form may vary depending on the exact form and the type of service or medication being requested. However, generally, the following information is commonly required:
1. Patient Information: This includes the patient's full name, date of birth, gender, and contact information.
2. Healthcare Provider Information: This includes the name, address, phone number, and NPI (National Provider Identifier) of the healthcare provider requesting the prior authorization.
3. Prescription/Service Information: This includes details about the medication or service being requested, such as the drug name, strength, quantity, and frequency of use. For services, it may include the CPT (Current Procedural Terminology) code and a description of the service.
4. Diagnosis: The specific diagnosis or medical condition for which the medication or service is being requested should be provided.
5. Medical Necessity: The provider may need to provide documentation supporting the medical necessity of the requested medication or service. This can include clinical notes, test results, or other relevant information.
6. Insurance Information: The patient's insurance information, including their member ID, group number, and other relevant details, may be required.
7. Provider Signature: The form typically requires the signature and credentials of the healthcare provider submitting the prior authorization request.
It is important to consult with Molina or refer to their specific prior authorization form to ensure accurate and complete reporting of the required information.
How can I modify molina prior authorization form without leaving Google Drive?
Using pdfFiller with Google Docs allows you to create, amend, and sign documents straight from your Google Drive. The add-on turns your molina prior authorization form michigan into a dynamic fillable form that you can manage and eSign from anywhere.
How do I make changes in molina authorization form?
With pdfFiller, it's easy to make changes. Open your molina medicaid prior authorization form in the editor, which is very easy to use and understand. When you go there, you'll be able to black out and change text, write and erase, add images, draw lines, arrows, and more. You can also add sticky notes and text boxes.
Can I create an electronic signature for signing my molina prior authorization form pdf in Gmail?
With pdfFiller's add-on, you may upload, type, or draw a signature in Gmail. You can eSign your molina prior authorization michigan form and other papers directly in your mailbox with pdfFiller. To preserve signed papers and your personal signatures, create an account.
Fill out your molina prior authorization form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Molina Authorization Form is not the form you're looking for?Search for another form here.
Keywords relevant to molina michigan prior authorization form
Related to molina imaging prior authorization
If you believe that this page should be taken down, please follow our DMCA take down process
here
.